Gut Health and Our Mental Health
This week, Wounded Birds Ministry welcomes Kathy Vincent to the flock! Kathy is a registered dietician, and this week shares with us amazing information on gut health and how it impacts our mental health. While Kathy focuses on depression in this article, anxiety and other mental illnesses are also impacted.
The Challenge
As the holidays approach, most of us will be around the typical holiday fare, including a lot of sweets, leading up to the ever popular New Year’s Resolutions and ditching the “bad foods” for a new diet that will surely transform us throughout the year.
We will be thinking of our favorite foods for Thanksgiving and Christmas get-togethers, relying on those that make us feel good or remind us of our childhood.
But how good do those sweets and comfort foods really make us feel?
There is seldom a shortage of stories about people overeating, trying not to gain weight throughout the holiday season, and feeling miserable after rushing from one family gathering to the next and having to eat multiple times to avoid hurting anyone’s feelings.
There is so much more at play, however. The holiday season is also a peak time for depression, not only as people may feel isolated from loved ones during this time, but financial stressors tend to overwhelm a majority of consumers, particularly when credit card bills start arriving.
Depression Is a Real and Growing Concern
The Centers for Disease Control and Prevention report that nearly 10% of Americans battle some type of depression, and since the World Health Organization estimates that in the next two years (by 2020), depression will be the 2nd-highest ranking disease worldwide, it demands a closer look at anything we can do to ease that burden.
[Editor’s Note: These stats are in reports available on their respective websites; I’m unable to link directly to them here.]
The last several decades have seen a steady increase in multiple diseases, including depression. With this rise, the quality of our diets has maintained a steady decline.
The Rise of Processed Foods Has Changed Our Moods
Since WWII, processed foods have become a mainstay throughout America’s kitchens, giving us a nutrient profile weak in fiber, antioxidants, omega-3 fatty acids, and increasing our consumption of inflammatory foods, refined sugar, and excess calories.
Inflammation and gut health are two areas that have begun receiving more attention – and with good reason. They are directly impacted by the foods we eat and the beverages we drink.
In turn, our brain health is affected, making it essential for those affected by or at risk for mental health disorders to adopt a lifestyle that reduces inflammation and improves gut health.
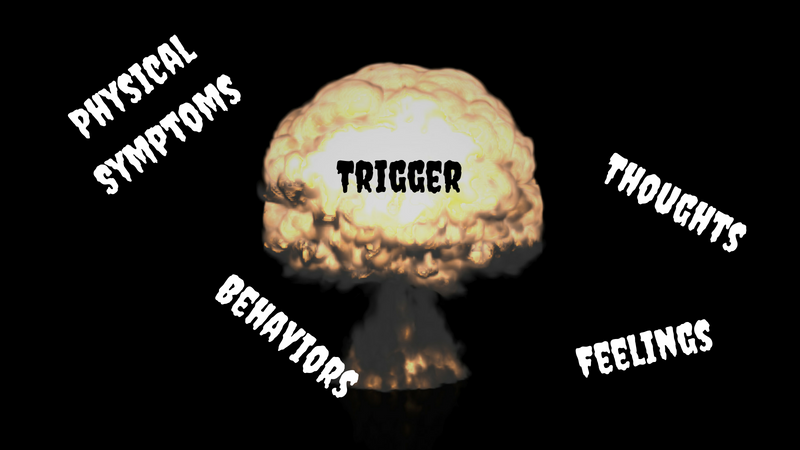
Inflammation is a natural process that ideally is short-lived to aid in healing the body after injury or other insults. But when it becomes chronic (usually as a result of multiple stressors), brain health and overall mood may deteriorate.
Nutrition Deficits Are Negatively Impacting Our Gut Health
Nutrient deficits from a poor quality diet, compounded with pro-inflammatory foods, provide the perfect recipe for chronic inflammation and for upsetting the gut microbiome, which has been called the body’s “second brain.”
Serotonin, an important neurotransmitter that plays a massive role in positively affecting mood, is primarily manufactured in the gut. In fact, 80-90% of serotonin is thought to be produced in the gut, so if gut health is not being protected, there becomes a higher risk for developing mood disorders and/or a greater struggle to overcome them.
What is involved with assessing gut health? A health professional may ask you questions about digestion, reactions to certain foods, and elimination functions such as constipation or frequency of bowel movements.
In addition to poor diet, food allergies/intolerances and medications (antibiotics, nonsteroidal anti-inflammatory medications, or NSAIDs, antacids, proton pump inhibitors) all may affect digestion and absorption of nutrients and can promote gut health dysfunction. Interestingly, the gut bacteria of a vegetarian is completely different from the gut bacteria of an omnivore!
Let’s take a closer look at each of the dietary components that affect inflammation and gut health.
Key Dietary Components Affecting Gut Health
Fiber
While a large number of people are concerned about getting enough protein (97% of the population receives adequate protein), only 3% of the population is getting enough fiber!
Fiber is the primary nutrient to feed your gut microbiota, producing short-chain fatty acids like butyrate, which is beneficial for the brain. Your immune system largely relies on the bacteria in your intestinal tract, so it’s important to feed the good bacteria and weed out the harmful bacteria.
Fiber is found only in plant foods, so look for whole grains, nuts, seeds, dried beans, fruits, and vegetables for this critical nutrient.
Antioxidants
By now, you have likely heard about free radicals and antioxidants. Free radicals, a byproduct of oxidative stress, can damage artery walls, promote inflammation, and negatively impact the brain and nervous system as a whole when left unchecked.
Antioxidants, such as Vitamins C and E, flavonoids and carotenoids, are found in a wide range of foods, but primarily plant foods, and play a vital role in neutralizing the destructive free radicals.
Are you seeing a pattern thus far? Numerous studies show that healthy plant-based diets all over the world are inversely associated with depression and mental health disorders.
Omega-3 Fatty Acids
There are three types of omega-3 fatty acids: Docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), and alpha-linolenic acid (ALA).
The research in this area reflects the positive effects of omega-3 fatty acids on mental health disorders, including depression from multiple causes, bipolar depression, and schizophrenia.
They are critical for a well-functioning central nervous system and are thought to be responsible for the health and well-being of populations in cold areas of the world that have unusually low depression rates.
DHA and EPA are both found in cold-water fish such as salmon, tuna, and mackerel, but it’s crucial to get wild-caught fish, as their diet in the wild is the primary source of these critical nutrients.
Aim to eat fish twice/week for the best benefit.
ALA, while it does not directly affect mood, is found in plants foods such as walnuts, hemp hearts, chia seeds, flaxseed, pumpkin seeds, and purslane. A small amount of ALA is converted by the body into EPA and DHA. These are especially delicious and convenient consumed in smoothies, atop cereal and salads, or combined to make granola.
As you know, nutrition is not the be-all and end-all of good mental health care. Exercise and adequate sleep are other important considerations in controlling mood disorders.
Final Tips
It’s important to take a close look at your normal eating patterns to identify trends and areas that can be improved for good gut health. Keeping a food journal may be particularly helpful.
Look for ways to add in a wide variety of plant foods; menu plan as much as possible; eliminate sugar-sweetened beverages and replace with water; eat cold-water, fatty fish twice/week; and opt for whole grains and high fiber foods. Each of these will help you modify your gut health and stabilize your moods.
Take some of these healthier options to family events during the holidays to guarantee the availability of healthful foods, and start new traditions with your family and friends.
They may be needing an extra boost of mood-enhancing nutrients, too!
Kathy Vincent
Registered Dietician
What do you think of gut health? What’s one way you’ve considered modifying your nutrition to help you manage your symptoms? How has it helped?
Looking for daily inspiration and community? Join our warm and supportive Facebook group!